A systematic review and standardized clinical validity assessment of male infertility genes
Manon S. Oud, Ludmila Volozonoka, Roos M. Smits, Lisenka E. L. M. Vissers, Liliana Ramos, Joris A. Veltman, 13.03.2019
Abstract
STUDY QUESTIONWhich genes are confidently linked to human monogenic male infertility?SUMMARY ANSWEROur systematic literature search and clinical validity assessment reveals that a total of 78 genes are currently confidently linked to 92 human male infertility phenotypes.WHAT IS KNOWN ALREADYThe discovery of novel male infertility genes is rapidly accelerating with the availability of next-generating sequencing methods, but the quality of evidence for gene–disease relationships varies greatly. In order to improve genetic research, diagnostics and counseling, there is a need for an evidence-based overview of the currently known genes.STUDY DESIGN, SIZE, DURATIONWe performed a systematic literature search and evidence assessment for all publications in Pubmed until December 2018 covering genetic causes of male infertility and/or defective male genitourinary development.PARTICIPANTS/MATERIALS, SETTING, METHODSTwo independent reviewers conducted the literature search and included papers on the monogenic causes of human male infertility and excluded papers on genetic association or risk factors, karyotype anomalies and/or copy number variations affecting multiple genes. Next, the quality and the extent of all evidence supporting selected genes was weighed by a standardized scoring method and used to determine the clinical validity of each gene–disease relationship as expressed by the following six categories: no evidence, limited, moderate, strong, definitive or unable to classify.MAIN RESULTS AND THE ROLE OF CHANCEFrom a total of 23 526 records, we included 1337 publications about monogenic causes of male infertility leading to a list of 521 gene–disease relationships. The clinical validity of these gene–disease relationships varied widely and ranged from definitive (n = 38) to strong (n = 22), moderate (n = 32), limited (n = 93) or no evidence (n = 160). A total of 176 gene–disease relationships could not be classified because our scoring method was not suitable.LARGE SCALE DATANot applicable.LIMITATIONS, REASONS FOR CAUTIONOur literature search was limited to Pubmed.WIDER IMPLICATIONS OF THE FINDINGSThe comprehensive overview will aid researchers and clinicians in the field to establish gene lists for diagnostic screening using validated gene–disease criteria and help to identify gaps in our knowledge of male infertility. For future studies, the authors discuss the relevant and important international guidelines regarding research related to gene discovery and provide specific recommendations for the field of male infertility.STUDY FUNDING/COMPETING INTEREST(S)This work was supported by a VICI grant from The Netherlands Organization for Scientific Research (918-15-667 to J.A.V.), the Royal Society, and Wolfson Foundation (WM160091 to J.A.V.) as well as an investigator award in science from the Wellcome Trust (209451 to J.A.V.).PROSPERO REGISTRATION NUMBERNone.
OUD, Manon S., et al. A systematic review and standardized clinical validity assessment of male infertility genes. Human Reproduction, 2019, 34. Jg., Nr. 5, S. 932-941.
Publication: https://doi.org/10.1093/humrep/dez022
 Disclaimer
Disclaimer
The publication A systematic review and standardized clinical validity assessment of male infertility genes by Manon S. Oud, Ludmila Volozonoka, Roos M. Smits, Lisenka E. L. M. Vissers, Liliana Ramos, Joris A. Veltman is published under an open access license: http://creativecommons.org/licenses/by/4.0/. Granted rights: Share - copy and redistribute the material in any medium or format and Adapt - remix, transform, and build upon the material for any purpose, even commercially.
Curation by the MFGA team Relevant data sets presented in the publication have been identified. If possible, annotations (title, general information, conditions, processed tissue types and processed cell types) have been added based on information from the publication. Data tables and images that provide a good overview on the publication's findings on the data set have been extracted from the publication and/or supplement. If not stated otherwise, images are depicted with title and description exactly as in the publication. Tables have been adjusted to the MFGA table format. Conducted adjustments are explained in the detailed view of the tables. However, titles and descriptions have been adopted from the publication.
Data set 1: Systematic literature search
Genome: Other
Species
| Species |
|---|
| human |
Images
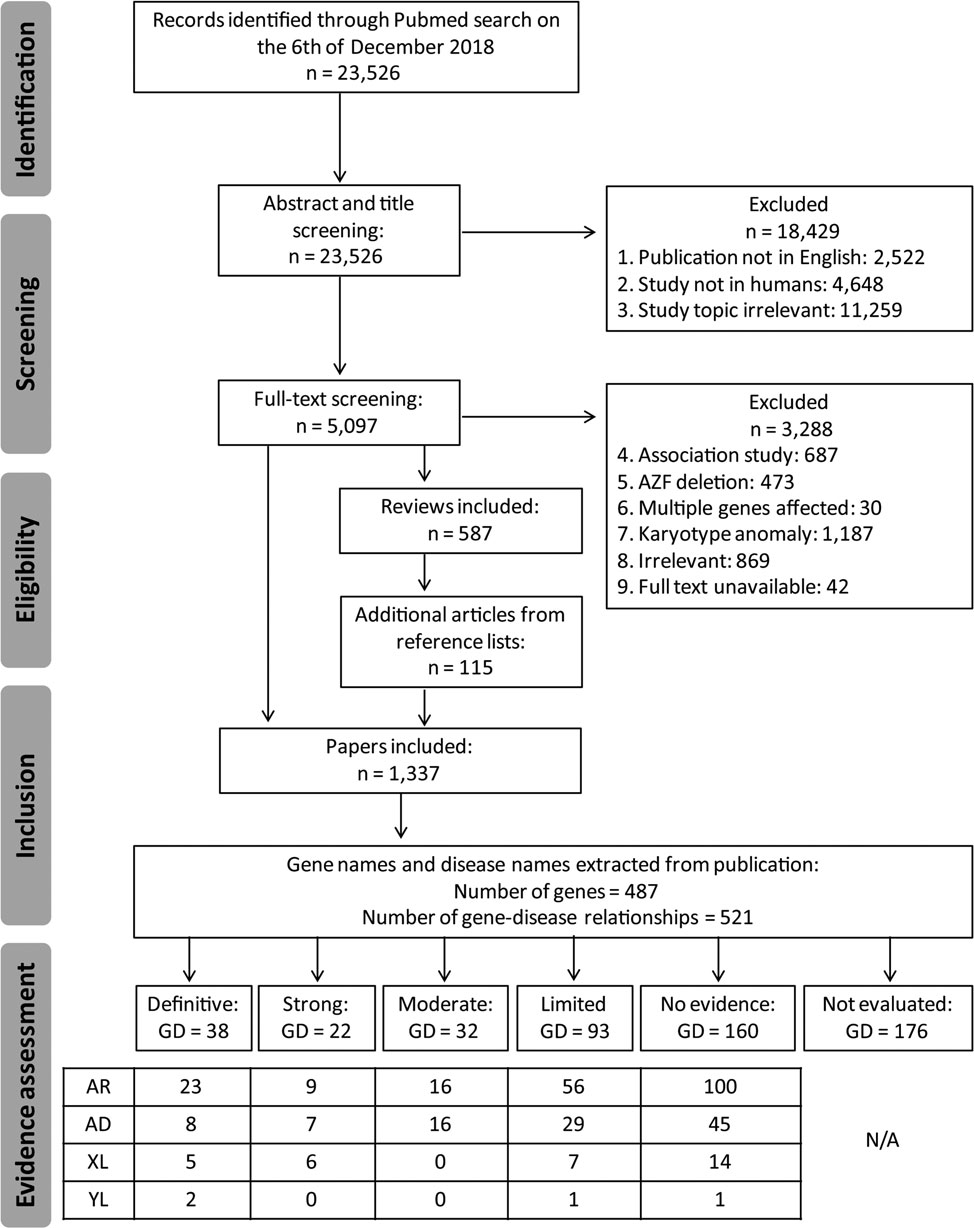
Figure 1: PRISMA flow chart showing our search and screening strategy to identify publications and genes eligible for clinical valid- ity assessment in male infertility
GD, gene–disease relationships; AR, autosomal recessive; AD, autosomal dominant; XL, X-linked; YL, Y-linked.
Licensed under: http://creativecommons.org/licenses/by/4.0/
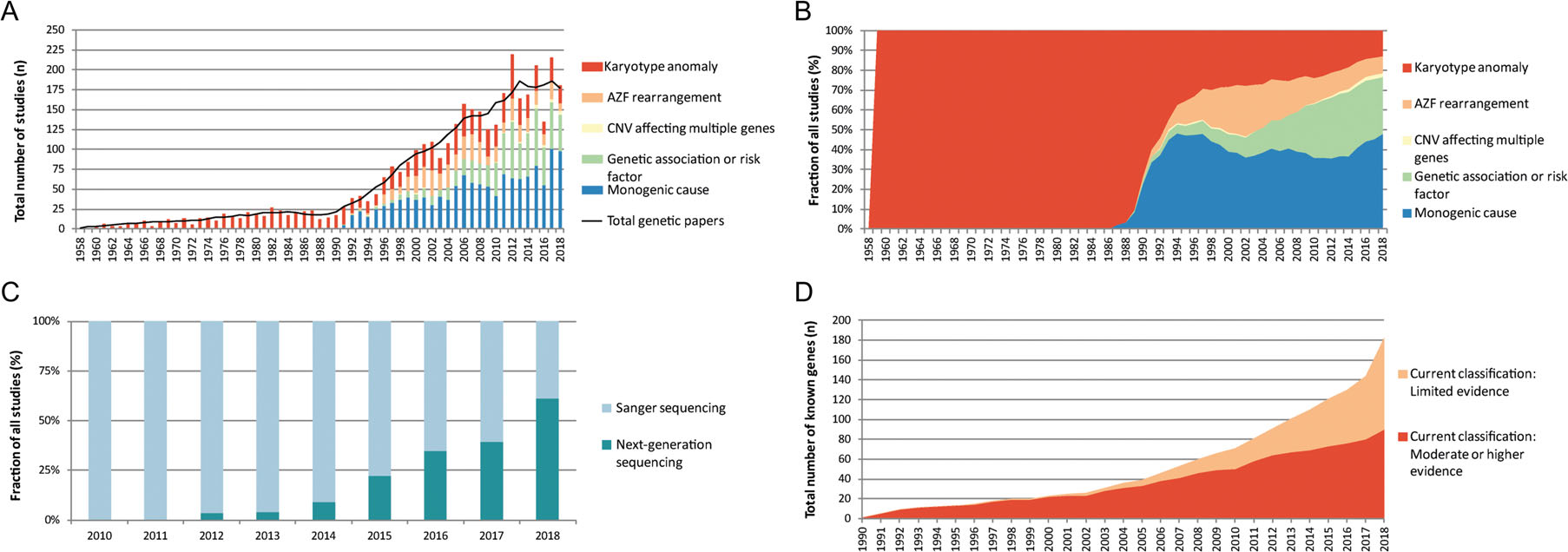
Figure 2: Genetic studies in male infertility between 1958 and 2018
(A) Graphical overview of genetic studies in male infertility. </br>(B) Graphical representation of type of genetic research in male infertility. </br>(C) The use of Sanger sequencing and next-generation sequencing for the discovery of genes in male infertility. </br>(D) Increase of genes linked to human male infertility. AZF, azoospermia factor; CNV, copy number variants.
Licensed under: http://creativecommons.org/licenses/by/4.0/
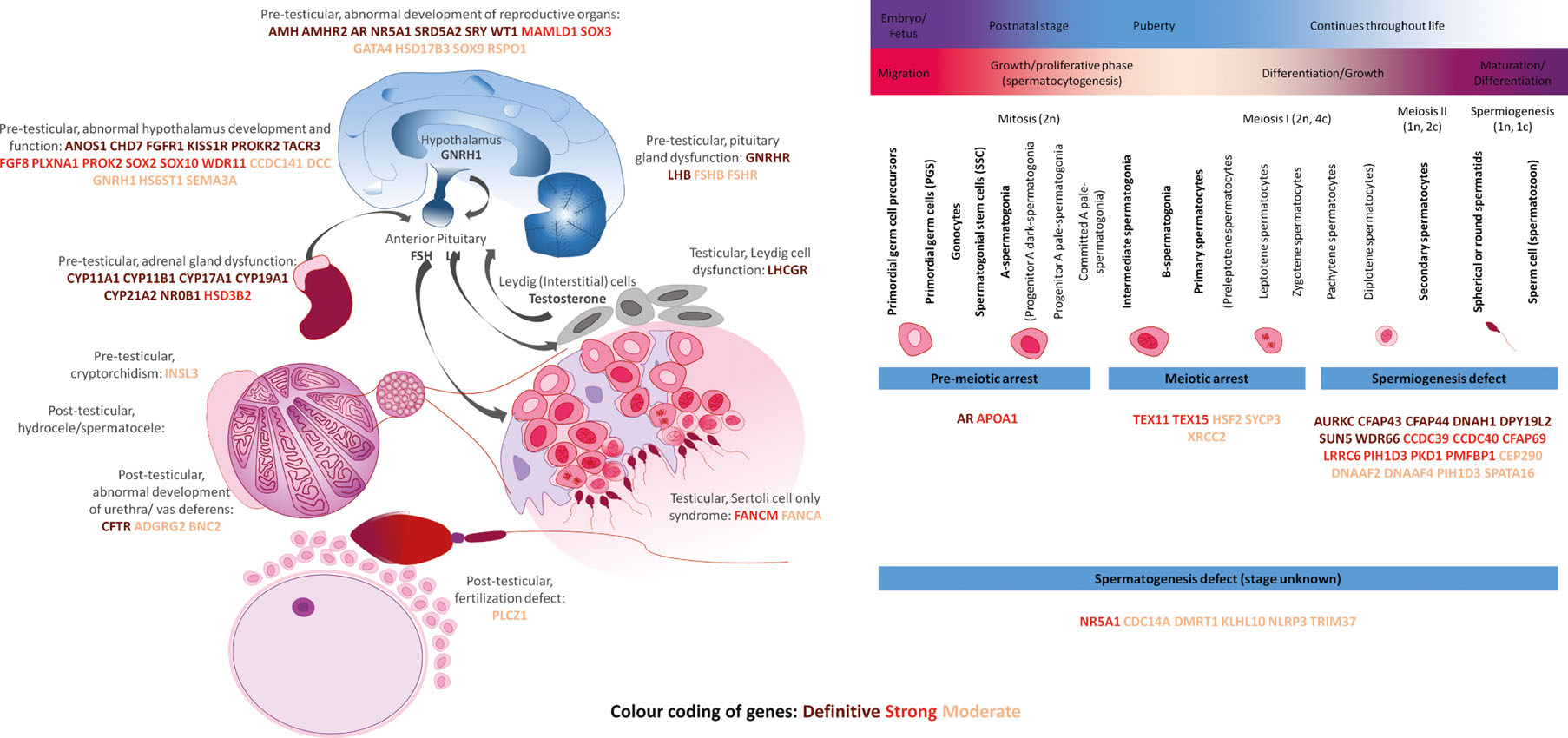
Figure 3: Biological overview of the genetics of male infertility
The color of each gene indicates the amount of evidence: Brown: Definitive; Red: Strong; Orange: Moderate. GnRHR: GnRH receptor, LHCGR: LHCG receptor. A list of gene names and definitions is available in Supplementary Table S9.
Licensed under: http://creativecommons.org/licenses/by/4.0/
Results
- Supplementary Table S5: Genes without potentially pathogenic variants described first
- Supplementary Table S6: Genes that could not be classified with the current method and available information. first
- Supplementary Table S9: Gene names and definitions of genes at least moderately linked to male infertility (Fig. 3). first
- Supplementary Table S4: Scoring sheet for genes with at least one potentially pathogenic variant described. first
